Why Continuous Glucose Monitoring is Important
By: Diana Isaacs, PharmD, BCPS, BC-ADM, CDCES, FADCES
What is Glucose?
Glucose is sugar in the bloodstream. Insulin serves as the key to let glucose into the cells for storage and energy. The body needs glucose for energy, but too much glucose can cause damage to the body’s organs over time. In people with diabetes, they either do not have enough insulin or there is insulin resistance leading to higher blood sugar levels.
How to Measure Blood Sugar Levels1,2,3
According to the American Diabetes Association, the goals for most people with diabetes are 80-130mg/dL in the morning before eating as well as in between meals, if more than 4 hours has passed since the last meal. It is normal for blood sugar to rise after eating. The goal is to keep it under 180mg/dL, 1-2 hours after the start of the meal, which is when blood sugar is expected to peak after eating. These targets may be adjusted depending on a person’s individual needs or risk of low blood sugar.
When blood sugar goes under 70mg/dL, this is considered low blood sugar or hypoglycemia. When it is above 180mg/dL, this is called high blood sugar or hyperglycemia. Another measurement term called “time in range” is used to describe the percent of glucose readings that are between 70-180mg/dL. The idea is that more time in range means a more consistent blood sugar level with less of highs and lows. The recommendation for most people with type 1 and type 2 diabetes (that are targeting an A1C of less than 7%) is to achieve a time in range of 70% or more. For people that are older or at higher risk of low blood sugar levels and have an A1C target of less than 8%, the target time in range is 50%.
Blood Sugar Targets for Most People with Diabetes
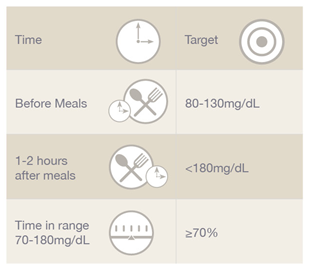
These targets may be adjusted depending on a person’s individual needs or risk of low blood sugar.
Symptoms of Low Blood Sugar
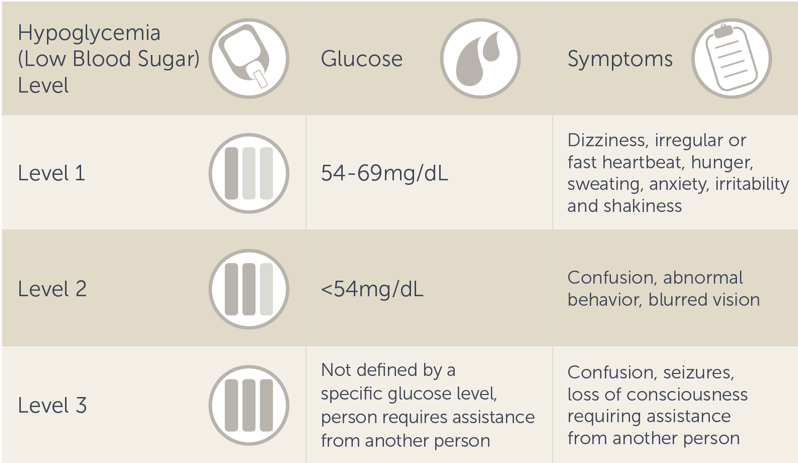
When a person produces too much insulin or gets too much medication, it can cause low blood sugar. Blood sugar between 54-69mg/dL is considered level 1 hypoglycemia. Typical symptoms of low blood sugar include:
- Dizziness
- Irregular or fast heartbeat
- Hunger
- Sweating
- Anxiety
- Irritability
- Shakiness
Some people may feel symptoms above 70mg/dL while others don’t feel symptoms until levels are even lower. Level 2 hypoglycemia is considered a blood sugar under 54mg/dL. This can lead to more severe symptoms such as confusion, abnormal behavior, and blurred vision because at this point the brain may not be getting enough glucose to function. When glucose gets too low this can lead to a person falling, having seizures or passing out. Level 3 hypoglycemia is when a person can’t think clearly or may have passed out, and needs the assistance of another person. This response is not defined by a specific glucose value.
Symptoms of High Blood Sugar4
When a person does not get enough insulin or medication to meet their body’s demands, it can lead to high blood sugar or hyperglycemia. There are many causes of hyperglycemia including untreated diabetes, not getting enough medication, eating too many carbohydrates, being less physically active, having excess weight, and genetic factors.
Typical symptoms of high blood sugar include:
- Extreme thirst
- The need to urinate often
- Blurry vision
- Increased hunger
- Feeling tired and weak
- Headache
Other symptoms can be severe and could include vomiting, confusion, shortness of breath and even coma.
Some symptoms of low blood sugar and high blood sugar can be similar, like blurred vision and drowsiness. Therefore, it is important to check blood sugar before treating.
Treatment of low and high blood sugar
Low blood sugar can be treated with fast-acting carbohydrate such as juice, regular soda, hard candies (not chocolate), or glucose tablets. People often ask, why not chocolate? This is because it contains fat, and fat will make the carbohydrate slower to absorb taking blood sugar longer to recover. It typically takes 15 minutes for blood sugar to rise. If a person is using insulin, it’s important not to take any insulin with the glucose treatment. If after checking blood sugar again in 15 minutes it’s still below 70mg/dL, the glucose intake can be repeated. Once blood sugar is above 70mg/dL, a person should continue to eat a more complete meal or snack that includes protein such as half a sandwich or peanut butter and crackers. If a person is passed out or unable to consume food or liquids, glucagon can be used as an emergency treatment. Glucagon is available as either an injection or nasal powder. Every person with diabetes at risk of low blood sugar should have a prescription for glucagon.
Treatment of high blood sugar is trickier as it takes longer for a high blood sugar to come back into target range. Some strategies include drinking a lot of water or sugar free beverages. Taking a walk is also a great way to bring down a high blood sugar, however caution should be used when exercising intensely with high blood sugar as it can increase levels. In addition to exercise and fluids, those taking insulin have an option to take a correction dose to lower blood sugar. A person who recently injected insulin with a meal must be cautious as the insulin can still be working in the body for several hours and may lead to low blood sugar. It’s important to talk with your healthcare team to determine what is best for you to treat high or low blood sugar.
If blood sugar levels are consistently high or low, your healthcare team may be able to introduce additional strategies such as modifying your meal plan, physical activity routine, and/or adjusting your medication regimen.
Importance of Monitoring Blood Glucose Levels5
Monitoring blood sugar helps to determine if you are meeting your glucose targets which helps to reduce the unpleasant symptoms of high and low blood sugar, and avoid long-term diabetes complications. It is helpful to remember that the numbers are neither good nor bad. They are simply information used to help you learn what is working well and identify areas for improvement in your diabetes management.
Blood sugar monitoring is important because A1C tests are only done every 3-6 months and reflect an average. Someone with an A1C in target could still have a lot of high and low blood sugar readings. That’s the value and power of blood sugar monitoring. How often you check your blood sugar should be determined by you and your healthcare team. Generally, people with type 1 diabetes or that take multiple daily injections of insulin or use an insulin pump, should check their blood sugar more frequently. They may check their blood sugar level before all meals & snacks, at bedtime, prior to exercise, prior to performing critical tasks like driving or anytime they may suspect low blood sugar including after treating low blood sugar until blood sugar has returned to 70mg/dL or higher. This can add up to 6-10 times/day, or can be done automatically through continuous glucose monitoring (CGM). For people with type 2 diabetes that don’t take insulin or just take insulin once daily, monitoring blood sugar can help when adjusting the meal plan, physical activity or medications. For example, a person with type 2 diabetes, may check once or twice per day alternating before meals and at bedtime, although some people choose to check more often.
One strategy in glucose monitoring is to start by checking blood sugar levels before meals to see if you are achieving your targets. Once readings before a meal are at the target, you can check your blood sugar before a meal and again 1-2 hours after to see how that food directly affected your blood sugar level – this is called paired readings and can be tried with different meals and when introducing new activities.
Simply collecting numbers is not useful unless some type of action is also taken. Therefore, it is important to share the information with your healthcare team and regularly meet with a diabetes care and education specialist to learn how to take action and improve the time you spend in target range.
42 Factors that Affect Blood Sugar6
It is understood that there are 42 factors that affect blood sugars and that people may respond differently to these factors. For example, a cup of black coffee with no sugar or milk in it, may actually cause someone’s blood sugar to rise while other people may have no response. To know how you uniquely respond, check your blood sugar before, during and after consumption. Alternatively, a continuous glucose monitor (CGM) could be worn to directly calculate the effects. Another example is physical activity. For many people light exercise like walking will lower blood sugar, but for some it has little effect. High intensity exercise like running can actually cause some people’s blood sugar to go down, but for some, it will actually go up. The time of day, level of fitness and training, and the amount of sleep you got the night before can all play a role in this. Tracking the data from blood sugar monitoring (BGM) is a valuable way to learn about yourself.
Monitoring Glucose with a CGM or BGM7,8,9
Blood glucose meters provide a blood sugar reading in a moment of time. If your blood sugar is rising or falling rapidly, BGM will often be more accurate in that moment. The use of a CGM requires wearing a sensor that checks blood sugar levels every 1-5 minutes, depending on the device. Continuous glucose monitoring provides more data points and helps to ease the burden of daily management. The decision to use CGM instead of BGM should be determined with your healthcare team. Though cost and insurance coverage of CGM devices can sometimes be a barrier, there is an option to use a professional CGM, which is owned by the clinic and worn by the person with diabetes on a short-term, as-needed basis, up to 14 days, and typically 2-4 times per year. Of course, you should check with your insurance plan first to confirm your options.
There are many benefits to blood sugar monitoring, particularly as you learn how your body uniquely responds to different factors. Blood sugar monitoring can help you achieve your glucose targets, increase your time in range, and feel your best while avoiding potential long-term complications from diabetes.
References:
1 American Diabetes Association: Glycemic Targets: Standards of Medical Care in Diabetes-2020 Diabetes Care 2020;43(Suppl. 1):S66–S76
2 Cleveland Clinic Last accessed August 31, 2020
3 Battelino T, Danne T, Bergenstal RM et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations from the International Consensus on Time in Range. Diabetes Care published online June 8, 2019
4 https://www.mayoclinic.org/diseases-conditions/hyperglycemia/symptoms-causes/syc-20373631 Last accessed September 9, 2020
5 Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm-2020 Executive Summary. Endocrine Practice. Vol. 26. No.1 January 2020.
6 https://diatribe.org/42factors Last accessed August 25, 2020
7 Cappon G, Vettoretti M, Sparacino G, Facchinetti A. Continuous Glucose Monitoring Sensors for Diabetes Management: A Review of Technologies and Applications. Diabetes Metab J 2019;43:383-397.
8 Kruger DF. Edelman SV, Hinnen DA, Parkin CG. Reference Guide for Integrating CGM into Clinical Practice. The Diabetes Educator. Volume 45, Supplement 1, February 2019
9 American Diabetes Association: Diabetes Technology: Standards of Medical Care in Diabetes- 2020 Diabetes Care 2020;43(Suppl. 1):S77–S88
US-POR-2000011








